Pain relief tablets, commonly known as analgesics, are a vital tool in modern medicine, used to alleviate discomfort from various conditions ranging from headaches to chronic illnesses. These tablets work by interfering with the body’s pain signaling mechanisms, helping to reduce or eliminate the sensation of pain. Pain itself is a complex and essential response that serves as the body’s alarm system, alerting us to potential harm and prompting protective actions. However, when pain becomes chronic or excessively severe, it can significantly impact an individual’s quality of life, making it difficult to perform daily activities or enjoy life.
The science behind pain relief tablets is rooted in their ability to target specific pathways in the nervous system that transmit pain signals to the brain. Different types of analgesics work in unique ways, depending on the source and intensity of the pain. Some block the production of chemicals that cause inflammation, while others interfere with the brain’s perception of pain. Understanding how these medications function can empower patients and healthcare providers to choose the most effective treatment, ensuring pain is managed safely and effectively while minimizing potential side effects.
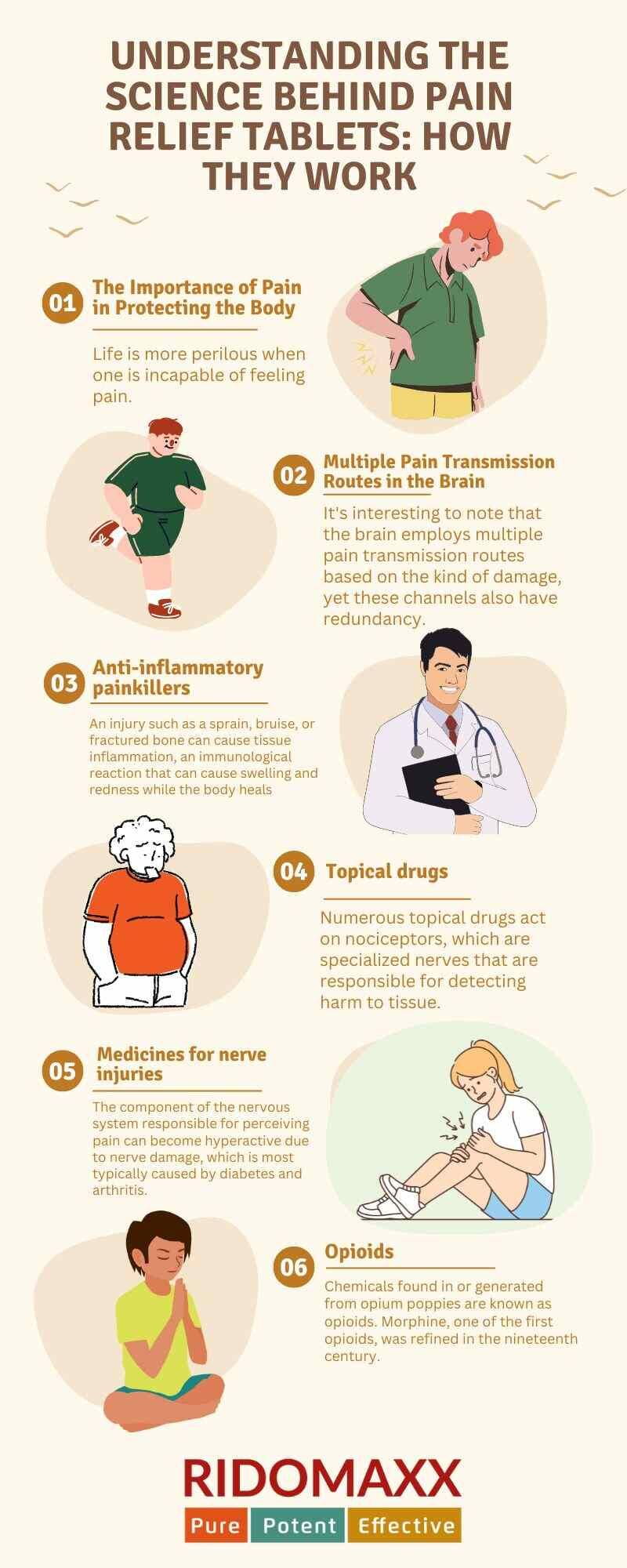
Here are some ways to understand the science behind pain relief tablets: How They Work
1. The Importance of Pain in Protecting the Body: Life is more perilous when one is incapable of feeling pain. Pain advises us to wait for the soup to cool, use a hammer more softly, or wear gloves when having a snowball battle in order to prevent harm. Individuals suffering from uncommon genetic illnesses that impair their sense of pain are unable to defend themselves against external hazards, which can result in fractures, skin damage, infections, and eventually a reduced lifespan.
Pain in these situations is a call to action for protection far more than just a feeling. However, excessively severe or prolonged pain can be incapacitating. How, then, does contemporary medicine lessen the call? This is a question that we, along with other researchers, have attempted to address as neurobiologists and anesthesiologists who specialize in pain studies. Over the past few years, scientific understanding of how the body detects tissue damage and interprets it as pain has advanced significantly. It is now evident that there are several channels that alert the brain to damage to its tissue and trigger pain.
2. Multiple Pain Transmission Routes in the Brain: It’s interesting to note that the brain employs multiple pain transmission routes based on the kind of damage, yet these channels also have redundancy. More intriguingly, even though pain’s protective role is no longer required, these brain circuits change and intensify signals in cases of chronic pain and pain brought on by illnesses that impact nerves directly.
Analgesics function by targeting distinct segments of these pathways. But not all painkillers are effective for all kinds of pain. A perfect painkiller is hard to come by due to the multiplicity and redundancy of pain pathways. But in the interim, knowing how currently available painkiller’s function enables patients and healthcare professionals to utilize them to their fullest potential.
3.Anti-inflammatory painkillers: An injury such as a sprain, bruise, or fractured bone can cause tissue inflammation, an immunological reaction that can cause swelling and redness while the body heals. Nociceptor nerve cells, which are specialized nerve cells in the injury site, detect the inflammatory chemicals produced by the body and communicate pain signals to the brain.
Typical over-the-counter anti-inflammatory pain relievers function by reducing inflammation at the site of injury. These are especially helpful for musculoskeletal injuries and other inflammatory pain conditions, like arthritis. Nonsteroidal anti-inflammatories like ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin do this by blocking an enzyme called COX that plays a key role in a biochemical cascade that produces inflammatory chemicals. When the cascade is blocked, it is less inflammatory.
Aspirin, naproxen (Aleve), ibuprofen (Advil, Motrin), and other nonsteroidal anti-inflammatories work by inhibiting an enzyme called COX, which is essential to a biochemical cascade that generates inflammatory chemicals. By stopping the cascade, the body produces fewer inflammatory chemicals, which in turn send the brain fewer pain messages. Although acetaminophen (Tylenol), sometimes referred to as paracetamol, inhibits COX enzymes and has comparable pain-relieving properties to NSAIDs, it does not have the same anti-inflammatory effects.
Other COX inhibitors, corticosteroids, and, more recently, medications that target and inactivate the inflammatory molecules themselves are examples of prescription anti-inflammatory pills. Medication that blocks inflammatory molecules will have side effects and possible health hazards, such as irritating the stomach lining and impairing renal function, because these chemicals are engaged in vital physiological tasks beyond just signaling pain. Generally speaking, over-the-counter drugs are safe as long as the instructions on the bottle are faithfully followed. Prednisone is one of the corticosteroids that stops the inflammatory cascade early in the process, which is likely why it reduces inflammation so well. All of the chemicals in the cascade are found in almost every organ system; thus, long-term steroid use can have a number of health hazards that should be discussed with a doctor before beginning any treatment.
4.Topical drugs: Numerous topical drugs act on nociceptors, which are specialized nerves that are responsible for detecting harm to tissue. Lidocaine and other local anesthetics stop these nerves from communicating electrically with the brain.
Topical analgesics also target the protein sensors on the ends of other skin sensory neurons. Certain sensations, such as the cooling effect of menthol or the searing feeling of capsaicin, can be elicited by activating these proteins, and these sensations can reduce the intensity of pain by decreasing the activity of the damage-sensing nerves.
These topical treatments are most effective when applied to pain that is directly related to the skin because they act on the minuscule nerves in the skin. For instance, shingles infections can harm skin nerves, making them hyperactive and leading the brain to receive continuous pain signals. These pain signals can be attenuated by applying topical lidocaine or a high dosage of capsaicin.
5. Medicines for nerve injuries: The component of the nervous system responsible for perceiving pain can become hyperactive due to nerve damage, which is most typically caused by diabetes and arthritis. Even in the absence of tissue damage, these injuries set off a pain alert. In these circumstances, the most effective medications are those that reduce that alarm.
Antiepileptic medications, such as gabapentin (Neurontin), inhibit electrical signals in the nerves, suppressing the pain-sensing system. But gabapentin can also lessen nervous system activity in other areas, which could cause confusion and drowsiness. It is believed that antidepressants, such as duloxetine and nortriptyline, regulate pain pathways by elevating specific neurotransmitters in the brain and spinal cord; however, they may also change chemical signals in the gastrointestinal tract, which can cause an unsettled stomach.
6.Opioids: Chemicals found in or generated from opium poppies are known as opioids. Morphine, one of the first opioids, was refined in the nineteenth century. Since then, a wide range of morphine derivatives, both natural and synthetic, with different potencies and durations, have been used in medicine. Codeine, tramadol, hydrocodone, oxycodone, buprenorphine, and fentanyl are a few typical examples.
Opioids reduce pain by triggering the endorphin system in the body. Your body naturally creates endorphins, a kind of opioid that reduces signals of damage and causes feelings of euphoria, also known as the “runner’s high.” Opioids act on comparable targets in the body to enhance the effects of endorphins.
Opioids are frequently useless for treating neuropathic injuries and chronic pain, but they help lessen some types of acute pain, such as pain following surgery, musculoskeletal injuries like a broken leg, or cancer discomfort.
The gastrointestinal tract and the lungs are two organ systems where the body uses opioid receptors; therefore, constipation and perhaps fatal breathing suppression are among the risks and side effects. Long-term opioid use may also result in tolerance, which increases the amount of the drug needed to produce the same level of pain relief. Because of this, opioids are not meant for long-term usage and can become addictive. Because of these risks and negative effects, doctors carefully prescribe all opioids, which are classified as restricted medications.
Conclusion
Pain relief capsules play a vital role in modern healthcare, offering relief from various types of pain, whether acute or chronic. The effectiveness of these capsules is rooted in their ability to target and modulate specific pathways in the body’s nervous system, which are responsible for transmitting pain signals to the brain. By understanding the underlying mechanisms of how pain relief capsules work, both patients and healthcare providers can make informed decisions on the most suitable pain management strategies.
While no single pain relief capsule can address every type of pain due to the complexity and redundancy of pain pathways, knowledge of these pathways allows for more tailored and effective treatment plans. This understanding helps in selecting the right medication to address specific pain conditions, ultimately improving patient outcomes and quality of life. As research continues to advance, the hope is that more refined and targeted pain relief solutions will be developed, offering even greater precision in managing pain. Until then, the thoughtful use of existing pain relief capsules remains a cornerstone in the management of pain, providing much-needed comfort and allowing individuals to lead more active and fulfilling lives.

0 Comments